Rapid Sequence Intubation Etomidate
Etomidate
Etomidate is a drug increasingly used as an induction agent for
endotracheal intubation. It has the advantage of not causing
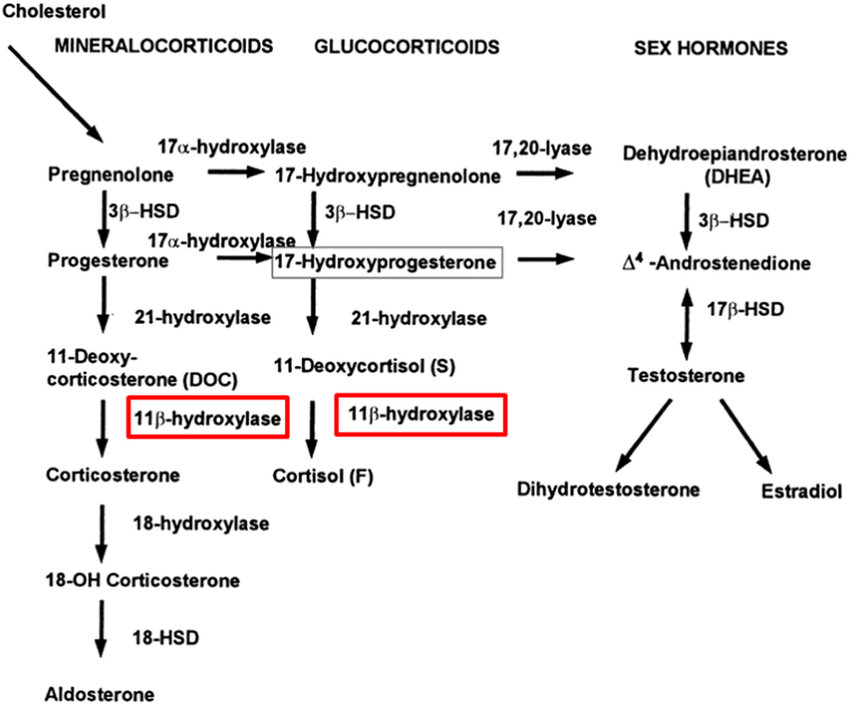
hemodynamic instability. This drug inhibits the 11β-hydroxylase
enzyme that converts 11-deoxycortisol into cortisol in the adrenal
gland and can cause AI. This adverse event has been described
with single-bolus and continuous infusions.
A 2015 Cochrane Library systematic review and meta-analysis
concluded that a single induction dose of etomidate was associated
with AI as evidenced by the results of ACTH stimulation testing.
The review also concluded that there is no strong evidence that
the use of single-dose etomidate increases mortality in critically
ill patients. Furthermore, etomidate was not found to be associated
with increased ICU length of stay, hospital length of stay, duration
of mechanical ventilation, or duration of vasopressor use.62 The
authors of this review judged the conclusions to be based on a
moderate quality of evidence and recommend that further trials
be designed to better answer this question.
Etomidate
Dose
0.3 mg/kg IV
(0.4 mg/kg sometimes cited, but 0.3 is standard)
Duration
Hypnosis lasts 10–15 minutes
Adrenal suppression
Structure resembles steroids
Can suppress cortisol synthesis transiently
Guidelines
❌ Old sepsis guidance: “avoid etomidate”
✅ Modern practice: acceptable single dose
If concern → check cortisol / give stress-dose steroids later
Bruder EA, Ball IM, Ridi S, Pickett W, Hohl C. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Cochrane Database Syst Rev. 2015 Jan 8;1(1):CD010225. doi: 10.1002/14651858.CD010225.pub2. PMID: 25568981; PMCID: PMC6517008.
Which of the following medications has not been shown to
cause adrenal insufficiency?
a. Ketoconazole
b. Propofol
c. Etomidate
d. Rifampin
Answer: b. Ketoconazle, etomidate, and rifampin have all been
documented to cause AI. Propofol may interfere with the actual
cortisol measurement. However, patients receiving propofol
maintain the response to the cosyntropin stimulation test.
Therefore the correct answer is choice b.
Administration of etomidate for rapid sequence intubation is associated with higher rates of adrenal insufficiency and mortality in patients with sepsis.
Chan CM, Mitchell AL, Shorr AF. Etomidate is associated with mortality and adrenal insufficiency in sepsis: a meta-analysis*. Crit Care Med. 2012 Nov;40(11):2945-53. doi: 10.1097/CCM.0b013e31825fec26. PMID: 22971586.
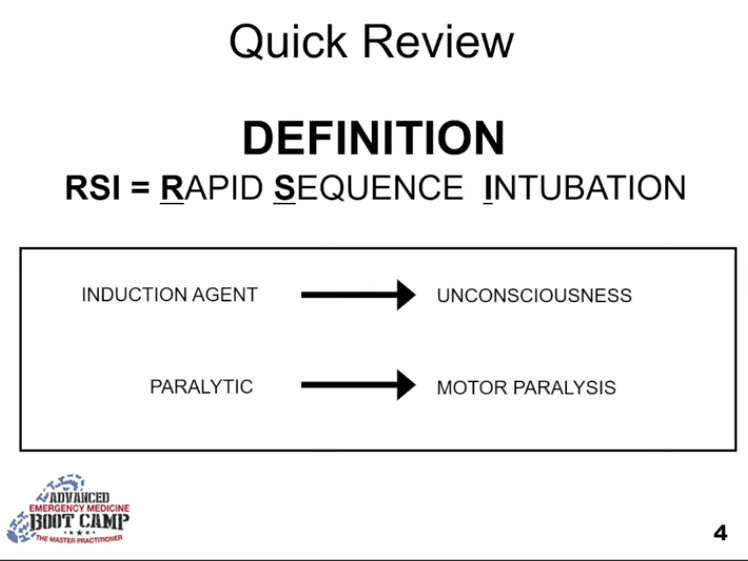
- reduce gastric contents, gastric aspiration and regurgitation, give sedation and paralytic in sequential order in pts that aren’t fasting
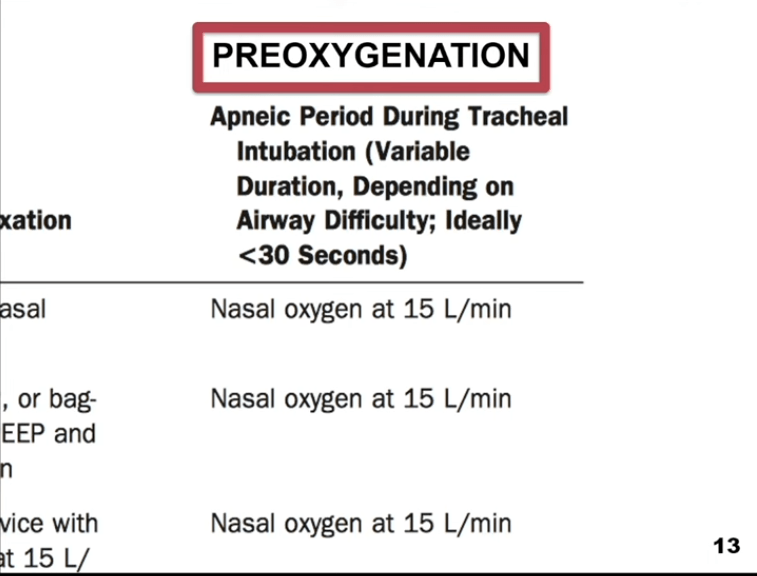
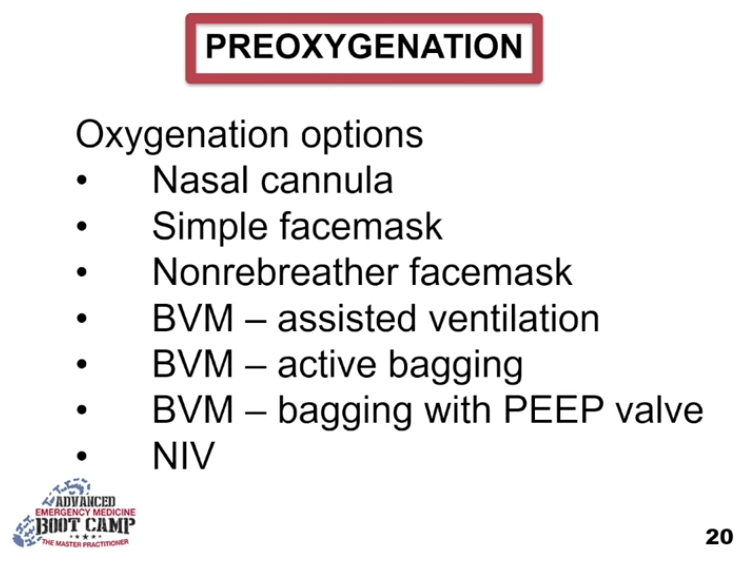
- Increase preoxygenation, increase safe apnea time longer preoxygenated / denitrogenate, throw nasal cannula on, 95% of is in lung, 5% in blood
- Paralysis to decrease catecholamine release that leads to increased ICP

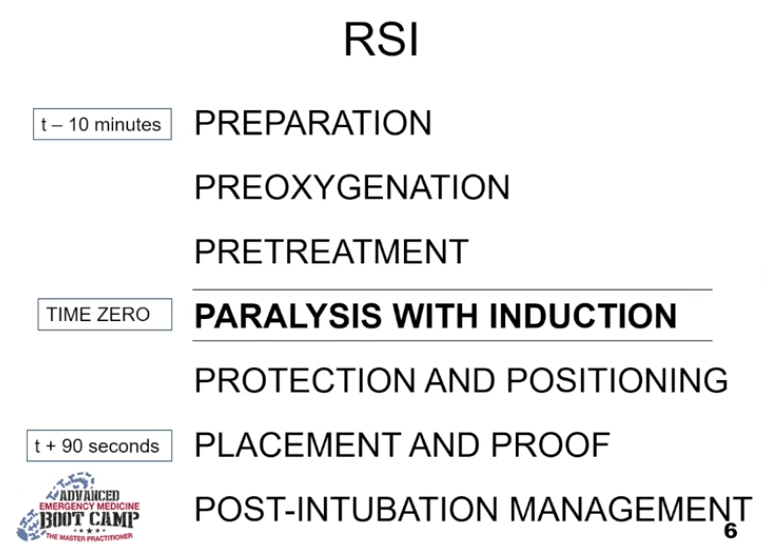
have removed pretreatment
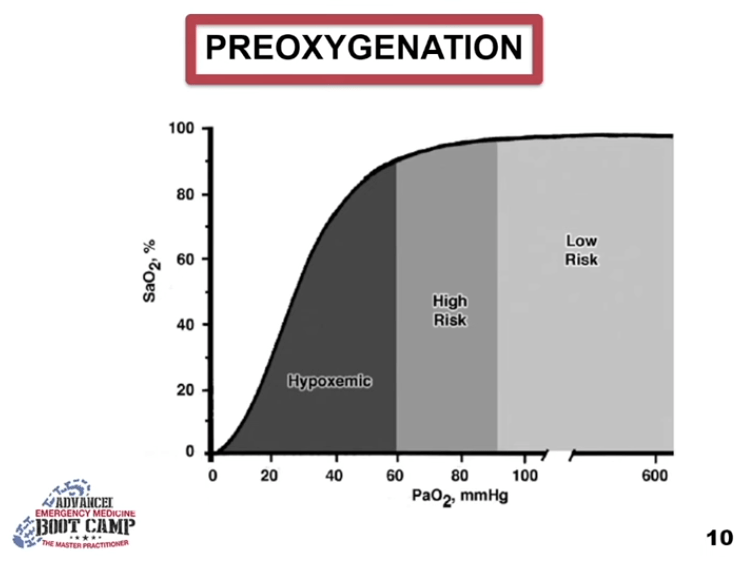
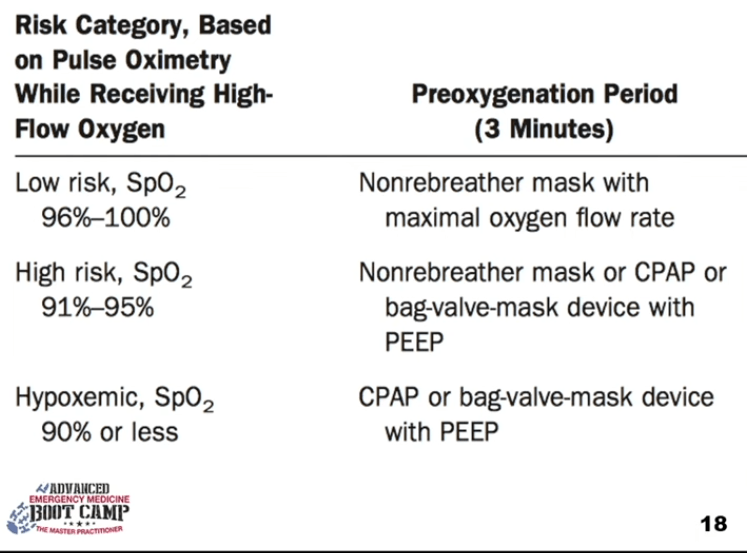
less than 90% drop off the cliff, want SaO2 as high as possible
Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012 Mar;59(3):165-75.e1. doi: 10.1016/j.annemergmed.2011.10.002. Epub 2011 Nov 3. PMID: 22050948.
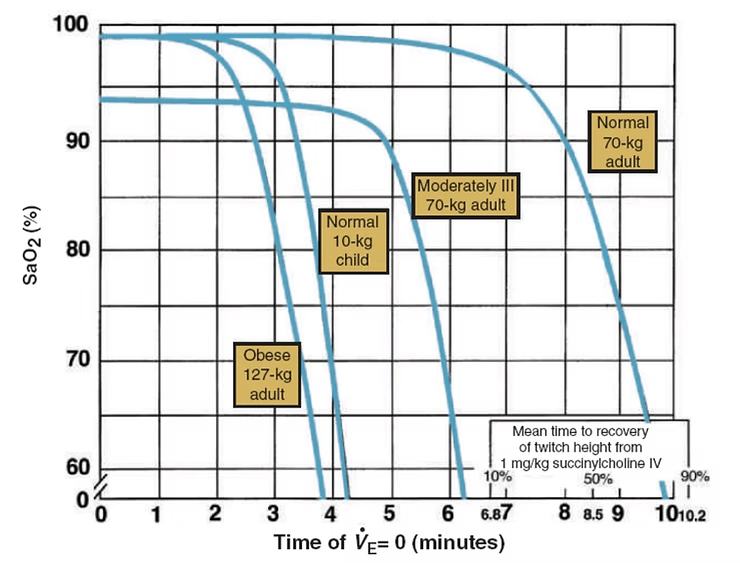
Benumof JL, Dagg R, Benumof R. Critical hemoglobin desaturation will occur before return to an unparalyzed state following 1 mg/kg intravenous succinylcholine. Anesthesiology. 1997 Oct;87(4):979-82. doi: 10.1097/00000542-199710000-00034. PMID: 9357902.
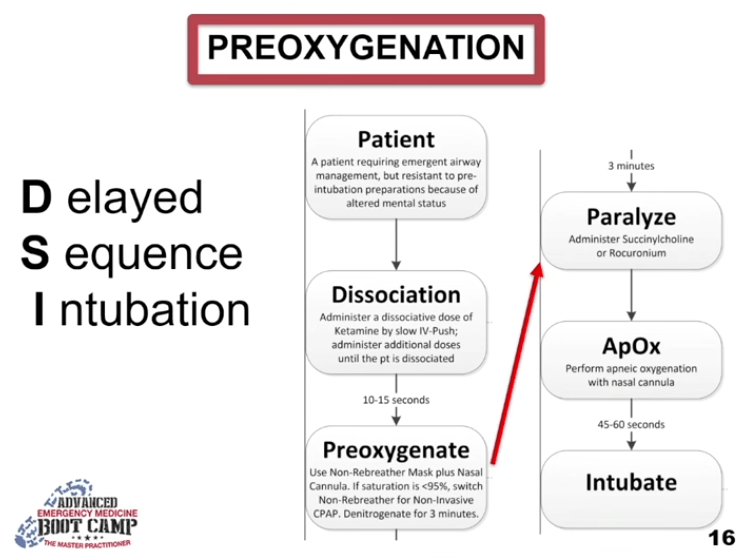
DSI delayed sequence intubation push sedative like ketamine, contain reflexes and dissociates 1mg/kg, additional 0.5mg/lkg
may need peep valve
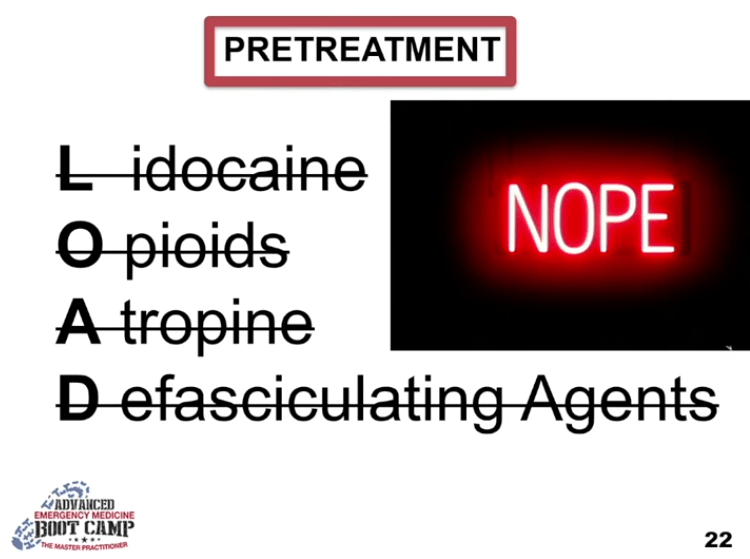
no pretreatment no more paralytics for fasciculations, lidocaine for ICP no evidence
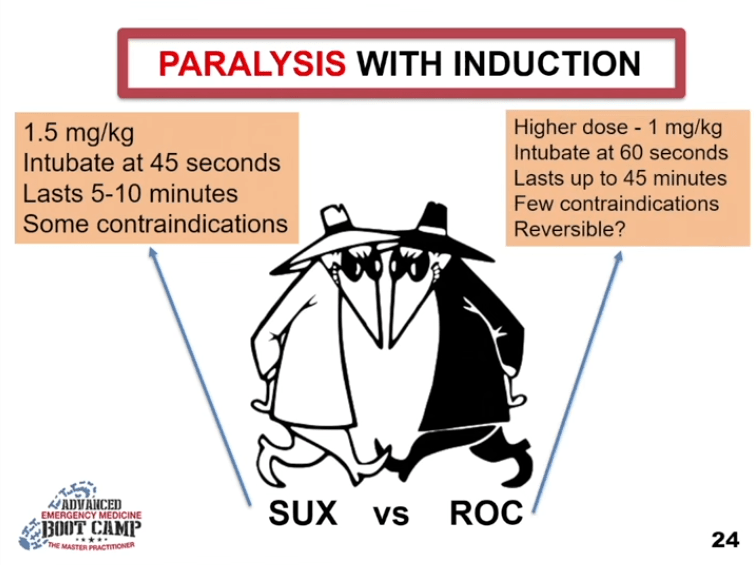
succinylcholine 1.5mg/kg intubate at 45 seconds, lasts 5-10 minutes, some contraindications hyperkalemia burns
Rocuronium higher dose 1mg/kg intubate at 60 seconds last 45 minutes, reversible? w/ sugammadex
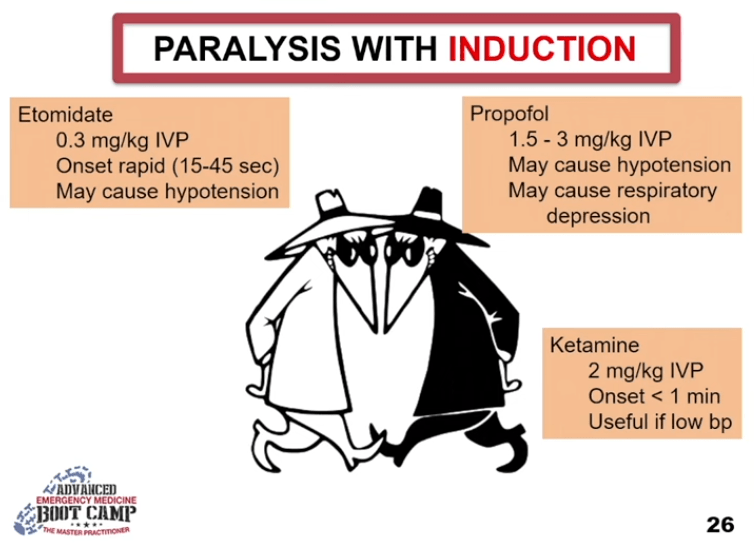
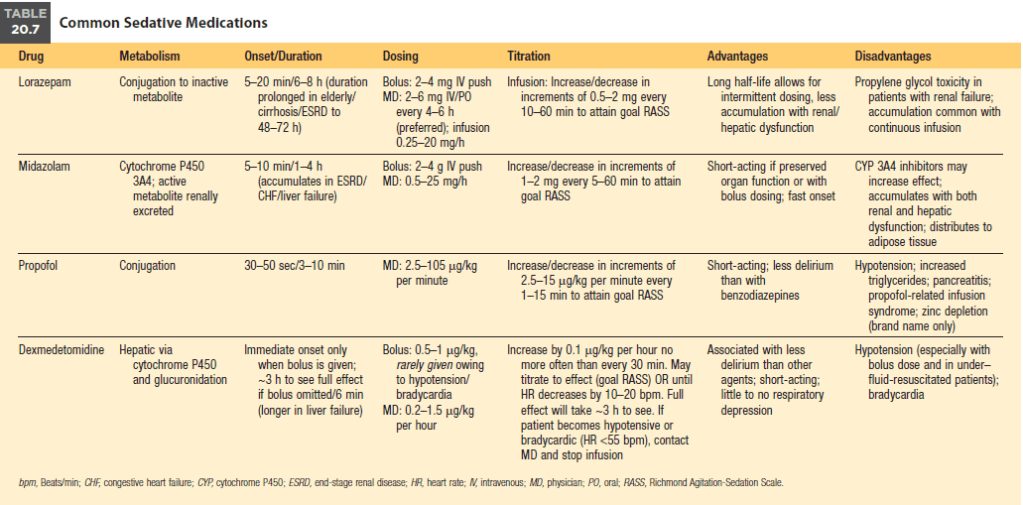
- etomidate 0.3mg/kg IVP, rapid onset 15-45 sec, may cause hypotension
- Propofol 1.5-3mg/kg IVP, may cause hypotension / respiratory depression
- Ketamine 2mg/kg IVP onset < 1 min useful if low bp
Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: a risk-benefit analysis. Ann Emerg Med. 2007 Dec;50(6):653-65. doi: 10.1016/j.annemergmed.2007.05.006. Epub 2007 Aug 3. PMID: 17681642.
Cricoid pressure is out
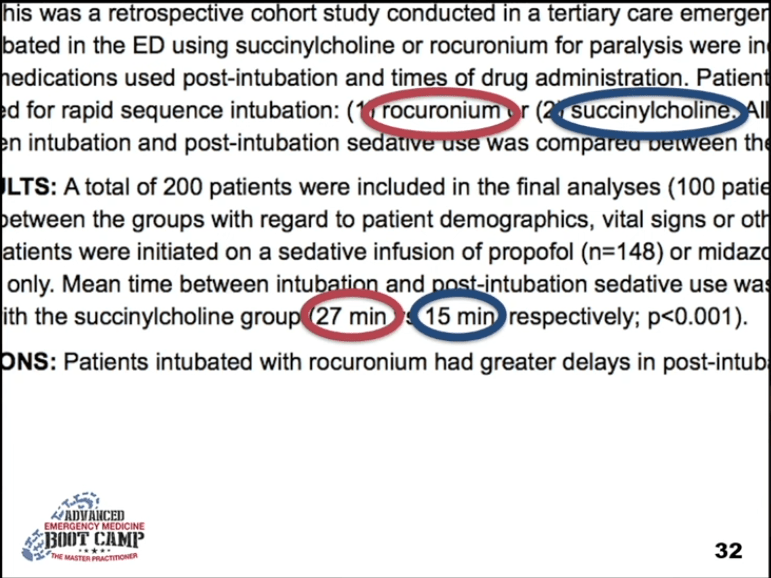
Watt JM, Amini A, Traylor BR, Amini R, Sakles JC, Patanwala AE. Effect of paralytic type on time to post-intubation sedative use in the emergency department. Emerg Med J. 2013 Nov;30(11):893-5. doi: 10.1136/emermed-2012-201812. Epub 2012 Nov 8. PMID: 23139098.
paralyzed patients can cry
RSI PREPARATION — CORE CONCEPTS
Preparation for RSI requires control over:
- {{c1::self}}
- {{c1::patient}}
- {{c1::others}}
- {{c1::environment}}
When communicating the airway plan, maintain a {{c2::“sterile cockpit”}} using a {{c2::call-and-response checklist}}.
🔹 RSI EQUIPMENT — SOAPME
SOAPME mnemonic stands for:
- S {{c3::Suction}} — at least one working suction, placed {{c3::between mattress and bed}}
- O {{c4::Oxygen}} — NRBM + BVM at {{c4::15 L/min}}, consider nasal prongs for {{c4::apneic oxygenation}}
- A {{c5::Airways}} — ET tube sizes: {{c5::7.5 most adults, 7.0 smaller females, 8.0 larger males}}
- P {{c6::Pre-oxygenation}} — {{c6::15 L/min NRBM}}
- M {{c7::Monitoring/Medications}} — cardiac monitor, pulse ox, BP cuff opposite IV, drugs drawn up
- E {{c8::End-tidal CO₂}}
ALWAYS have {{c9::surgical cricothyrotomy kit}} available during RSI.
🔹 RSI EQUIPMENT — O2 MARBLES
O₂ MARBLES mnemonic includes:
- O₂ {{c10::Oxygen masks and monitoring}}
- M {{c11::Airway adjuncts (OPA, NPA, LMA) + ask for help}}
- A {{c12::RSI drugs + resuscitation drugs}}
- R {{c13::BVM + bougie}}
- B {{c14::Laryngoscopes + LMA}}
- L {{c15::ET tubes + ETCO₂}}
- E {{c16::Suction + state airway plan}}
🔹 IDEAL RSI INDUCTION AGENT (DOES NOT EXIST)
An ideal RSI induction agent would:
- {{c17::Rapidly induce unconsciousness in one arm-brain circulation time}}
- {{c17::Provide analgesia}}
- {{c17::Maintain stable CPP and hemodynamics}}
- {{c17::Be immediately reversible}}
- {{c17::Have minimal side effects}}
🔹 INDUCTION AGENTS — DOSAGES
Ketamine dose (IV): {{c18::1.5–2 mg/kg IBW}}
Etomidate dose: {{c19::0.3–0.4 mg/kg TBW}}
Fentanyl dose: {{c20::2–10 mcg/kg TBW}}
Midazolam dose: {{c21::0.1–0.3 mg/kg TBW}}
Propofol dose: {{c22::1–2.5 mg/kg IBW + 0.4 × TBW}}
Thiopental dose: {{c23::3–5 mg/kg TBW}}
🔹 KETAMINE
Ketamine onset: {{c24::60–90 seconds}}
Ketamine duration: {{c24::10–20 minutes}}
Ketamine is preferred in RSI for:
- {{c25::Hemodynamic instability}}
- {{c25::Traumatic brain injury (does NOT increase ICP)}}
- {{c25::Reactive airway disease (bronchodilation)}}
Ketamine drawbacks include:
- {{c26::Increased secretions}}
- {{c26::Hypertension and tachycardia}}
- {{c26::Rare laryngospasm}}
- {{c26::Increased intra-ocular pressure}}
🔹 ETOMIDATE
Etomidate onset: {{c27::10–15 seconds}}
Etomidate is suitable for RSI except in:
- {{c28::Sepsis}}
- {{c28::Seizures}}
Major drawback of etomidate: {{c29::Adrenal suppression}}
🔹 PROPOFOL
Propofol onset: {{c30::15–45 seconds}}
Propofol duration: {{c30::5–10 minutes}}
Propofol drawbacks include:
- {{c31::Hypotension}}
- {{c31::Myocardial depression}}
- {{c31::Reduced cerebral perfusion}}
- {{c31::Pain on injection}}
🔹 FENTANYL
Fentanyl onset: {{c32::<60 seconds (max ~5 min)}}
High-dose fentanyl risk: {{c33::Chest wall rigidity}}
Fentanyl may be used as:
- {{c34::Sympatholytic premedication (TBI, SAH)}}
- {{c34::Modified RSI in cardiogenic shock}}
🔹 MIDAZOLAM
Midazolam is {{c35::NOT recommended}} for routine RSI due to:
- {{c35::Slow onset}}
- {{c35::Hypotension}}
- {{c35::Variable response}}
🔹 PARALYTICS — SUCCINYLCHOLINE
Succinylcholine dose: {{c36::1–2 mg/kg IV TBW}}
Onset: {{c36::45–60 seconds}}
Duration: {{c36::6–10 minutes}}
Absolute contraindications to succinylcholine include:
- {{c37::Hyperkalemia}}
- {{c37::Malignant hyperthermia}}
- {{c37::>5 days post burns/crush injury/neuromuscular disease}}
🔹 PARALYTICS — ROCURONIUM
Rocuronium RSI dose: {{c38::1.2 mg/kg IBW}}
Onset: {{c38::~60 seconds}}
Rocuronium advantage in CICV: {{c39::Provides immobility for cricothyrotomy}}
Reversal agent for rocuronium: {{c40::Sugammadex}}
🔹 PARALYTICS — VECURONIUM
Vecuronium onset: {{c41::120–180 seconds}}
Duration: {{c41::45–60 minutes}}
Vecuronium is {{c42::NOT recommended}} for RSI due to:
- {{c42::Slow onset}}
- {{c42::Prolonged paralysis}}
Importance of first pass intubation
The importance of first pass success when performing orotracheal intubation in the emergency department. AUSakles JC, Chiu S, Mosier J, Walker C, Stolz U SOAcad Emerg Med. 2013;20(1):71.
OBJECTIVESThe goal of this study was to determine the association of first pass success with the incidence of adverse events (AEs) during emergency department (ED) intubations.
METHODSThis was a retrospective analysis of prospectively collected continuous quality improvement data based on orotracheal intubations performed in an academic ED over a 4-year period. Following each intubation, the operator completed a data form regarding multiple aspects of the intubation, including patient and operator characteristics, method of intubation, device used, the number of attempts required, and AEs. Numerous AEs were tracked and included events such as witnessed aspiration, oxygen desaturation, esophageal intubation, hypotension, dysrhythmia, and cardiac arrest. Multivariable logistic regression was used to assess the relationship between the primary predictor variable of interest, first pass success, and the outcome variable, the presence of one or more AEs, after controlling for various other potential risk factors and confounders.
RESULTSOver the 4-year study period, there were 1,828 orotracheal intubations. If the intubation was successful on the first attempt, the incidence of one or more AEs was 14.2% (95% confidence interval [CI] = 12.4% to 16.2%). In cases requiring two attempts, the incidence of one or more AEs was 47.2% (95% CI = 41.8% to 52.7%); in cases requiring three attempts, the incidence of one or more AEs was 63.6% (95% CI = 53.7% to 72.6%); and in cases requiring four or more attempts, the incidence of one or more AEs was 70.6% (95% CI = 56.2.3% to 82.5%). Multivariable logistic regression showed that more than one attempt at tracheal intubation was a significant predictor of one or more AEs (adjusted odds ratio [aOR]= 7.52, 95% CI = 5.86 to 9.63).
CONCLUSIONSWhen performing orotracheal intubation in the ED, first pass success is associated with a relatively small incidence of AEs. As the number of attempts increases, the incidence of AEs increases substantially.ADDepartment of Emergency Medicine, University of Arizona, Tucson, AZ, USA. sakles@aemrc.arizona.edu PMID23574475
Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013 Jan;20(1):71-8. doi: 10.1111/acem.12055. PMID: 23574475; PMCID: PMC4530518.
Leave a comment